The Difference Between STDs And STIs Explained
STDs And STIs Are Not One In The Same: Here’s The Major Difference
Share the post
Share this link via
Or copy link
Source: BSIP / Getty
There are an estimated 20 million new cases of sexually transmitted infections every year in the United States, says the Office of Disease Prevention and Health Promotion. While some forms of prevention, including condoms, can reduce the risk of these infections, alarming data from Statista shows that many sexually active individuals do not use them. Access to information is one of the first lines of defense sexually active adults have against life-altering and life-threatening sexually transmitted diseases. Yet, many adults don’t know this one basic piece of knowledge: the differences between STDs and STIs.
The terms “STIs” and “STDs” are often used interchangeably, but they are far from one and the same. Getting clear on the language surrounding sexually transmitted infections and diseases – and how they are diagnosed and treated – can empower you in your medical journey, should you ever receive a diagnosis. So, when it comes to STDs and STIs, here’s what you need to know.
Love MadameNoire? Get more! Join the MadameNoire Newsletter
We care about your data. See our privacy policy.
STIs vs STDs

Source: Thana Prasongsin / Getty
Though many people use the terms interchangeably, STIs actually precede and can cause STDs. All STDs are the results of STIs. However, not all STIs turn into STDs. When diagnosed and treated early enough, STIs can go away and never turn into an STD. However, when left untreated, some STIs can cause damages to cells in the body that ultimately disrupt important bodily processes. Below are some of the most common types of STIs and the STDs they can develop into.
- HIV and AIDS. HIV is the infection that, when left untreated, can turn into AIDs. However, not everyone diagnosed with HIV will get AIDS. It is critical that those at risk of HIV get tested regularly. Hiv.gov reports that one in seven individuals with HIV do not know they have it. Early diagnosis of HIV can reduce the chances that the infection turns into AIDS.
- Chlamydia and pelvic inflammatory disease. Chlamydia is the STI that can develop into pelvic inflammatory disease (PID). PID is an infection of one or multiple of the upper reproductive organs. It can lead to scarring of the fallopian tubes and an increased risk of an ectopic pregnancy.
- Gonorrhea and PID. Gonorrhea is another STI that can cause PID.
- Trichomoniasis and PID. Trichomoniasis can also lead to PID.
- Syphilis and tertiary syphilis. Syphilis is an STI that, when left untreated, can turn into tertiary syphilis. Tertiary syphilis is a form of late-stage syphilis that can lead to complications such as damage to the heart, blood vessels, eyes, liver, bones, joints, and even the brain.
- HPV and cancer. HPV is an STI that can turn into several types of cancer including cervical, anal, vaginal, vulvar, and penile.
What Causes STIs?

Source: Peter Dazeley / Getty
STIs are usually transmitted through sexual contact, including the exchange of bodily fluids or skin contact via the penis, vagina, anus or mouth. Most STIs are either caused by bacteria, a virus or a parasite.
HIV and HPV are caused by a virus. Chlamydia and syphilis are caused by bacteria. Trichomonaisis is caused by a parasite known as Trichomonas vaginalis.
Symptoms of STIs And STDs

Source: Grace Cary / Getty
If you are sexually active with multiple partners, do not use protection, or are in any way at risk of STIs, getting tested regularly is very important – even if you do not experience symptoms. In fact, most STIs do not cause symptoms. In many cases, by the time one experiences symptoms, the STI has already developed into an STD. Each STI and STD can cause different symptoms, but some to report to a doctor include:
- Unusual discharge
- Irregular periods or heavy bleeding
- Pain during sex
- Lower abdominal pain
- Pelvic pain
- Dark urine
- Sores, blisters or warts
- Flu-like symptoms, including rashes and fever
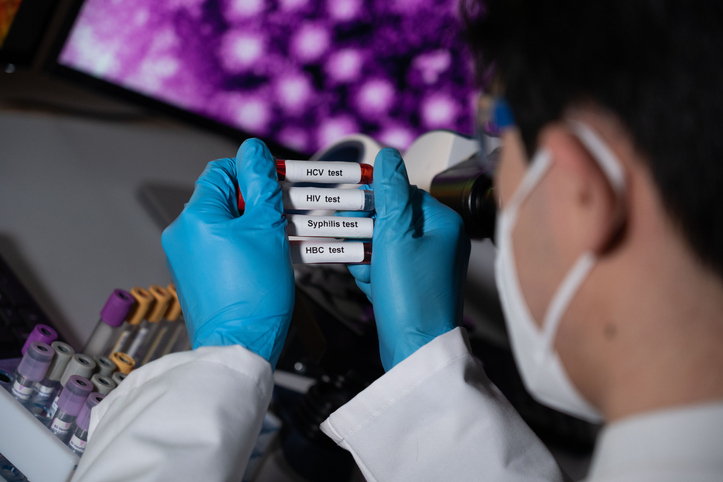
Diagnosing STIs vs STDs

Source: Lucas Ninno / Getty
Testing for STIs can happen through:
- Finger prick test
- Fluid sample from vagina, penis, anus or any sores
- Blood test
- Urine test
- Pelvic examination
If you test positive for an STI and your doctor suspects it has turned into an STD, further examinations can be required, including surgeries and more invasive procedures.
STD vs STI Treatment

Source: mikroman6 / Getty
It’s possible for some STIs clear up on their own, however they should not be left untreated. In most cases, doctors will recommend treatment to reduce the chances that an STI develops into an STD. Most STIs, including gonorrhea, syphilis and chlamydia, are treated with antibiotics. Chronic hepatitis B is treated with antiviral medications.
HIV, herpes and HPV cannot be cured. However, affected individuals can take antiviral medications for herpes and HIV. For those with herpes, these medications can shorten the length of outbreaks. For those with HIV, these medications can stop the virus from replicating.





